In today’s rapidly evolving healthcare landscape, digital health literacy has become an essential skill. As technology continues to shape the way we access and manage health information, being digitally literate can significantly impact our ability to make informed decisions about our well-being.
In today’s rapidly evolving healthcare landscape, digital health literacy has become an essential skill. As technology continues to shape the way we access and manage health information, being digitally literate can significantly impact our ability to make informed decisions about our well-being.
What is Digital Health Literacy?
Digital health literacy, sometimes referred to as eHealth literacy, is defined by the World Health Organization as the ability to seek, find, understand, and appraise health information from electronic sources, and apply the knowledge gained to address or solve a health problem. This includes the ability to find and evaluate health information online, access telehealth services, and communicate with healthcare providers electronically. As the internet becomes increasingly integrated into healthcare, digital health literacy enables individuals to navigate these resources effectively and make sound decisions about their health.
The Importance of Digital Health Literacy
Digital health literacy is closely linked to overall health literacy and access to technology. As the internet has become a primary source for health information, the ability to navigate this vast digital landscape is crucial. According to Pew Research, approximately 52% of American adults used the internet in 2000, compared to 89% in early 2018—a trend that is likely to continue rising. As more people turn to digital platforms for their health needs, digital health literacy enables individuals to:
- Access Reliable Health Information: The internet is filled with health-related content, but not all of it is accurate or trustworthy. Digital health literacy helps people discern credible sources from unreliable ones, ensuring they make decisions based on sound information.
- Manage Personal Health Records: Many healthcare providers offer online portals where patients can view their health records, schedule appointments, and communicate with their doctors. Being digitally literate allows patients to efficiently manage these resources.
- Use Health Apps and Wearables: Health apps and wearable devices provide valuable insights into personal health, from tracking physical activity to monitoring chronic conditions. Understanding how to use these tools effectively can lead to better health outcomes.
- Engage in Telemedicine: The rise of telemedicine has made it easier to consult healthcare providers remotely. Digital health literacy ensures that individuals can navigate virtual platforms, ensuring smooth communication and care.
Digital Health Literacy and Patient Safety
The impact of digital health literacy on patient outcomes is an emerging field of research. The ability to engage with digital resources is becoming increasingly necessary to find information, communicate with providers, manage appointments, access health records, and participate in health prevention and management interventions. However, low levels of digital health literacy can create barriers to accessing these essential services, leading to potential gaps in care and health equity.
There are many overlaps in the risk factors for low personal and digital health literacy, including age, race/ethnicity, socio-economic status, and educational status. These factors can exacerbate existing health disparities, making it even more important to address digital health literacy as part of broader efforts to promote health equity. As more research is conducted on the relationship between digital health literacy and outcomes, screening patients for digital health literacy using tools like the eHealth Literacy Scale (eHEALS) can help identify those who may benefit from targeted interventions. These interventions can increase patients’ ability to participate fully in the healthcare system and manage their health effectively.
Enhancing Your Digital Health Literacy
Improving digital health literacy is essential for staying informed and empowered in your healthcare journey. Here are some tips to help enhance your skills:
- Stay Informed: Keep up to date with the latest digital health tools and platforms. Familiarize yourself with reputable health websites, such as those provided by government health agencies or well-known medical institutions.
- Ask Questions: If you’re unsure about the information you find online, don’t hesitate to ask your healthcare provider. They can guide you to reliable sources and help you understand complex medical information.
- Use Online Health Portals: Take advantage of the online tools offered by your healthcare provider. These portals can be valuable resources for managing appointments, accessing lab results, and communicating with your care team.
- Evaluate Sources Critically: Learn to assess the credibility of online health information by checking the source, looking for evidence-based content, and being wary of sensational or overly simplistic claims.
The Impact of Digital Health Literacy on Health Outcomes
Higher levels of digital health literacy correlate with increased knowledge of health conditions and greater self-efficacy in managing chronic health conditions. Those with better digital health literacy are also more likely to access personal health records, which can lead to more informed health decisions and improved overall health outcomes. As the healthcare system continues to integrate more digital tools, enhancing digital health literacy will become increasingly important for ensuring equitable access to quality care.
In this digital age, being health-literate means not just understanding health information, but also being proficient in the digital tools that deliver that information. Equip yourself with these skills to navigate the digital healthcare landscape with confidence, ensuring your ability to manage your health and access the care you need effectively and safely.
References:
Centers for Disease Control and Prevention. (2022, July 20). eHealth literacy. Centers for Disease Control and Prevention. https://www.cdc.gov/healthliteracy/researchevaluate/eHealth.html
Seidel, E., Cortes, T., & Chong, C. (n.d.). PSNet. Digital Health Literacy. https://psnet.ahrq.gov/primer/digital-health-literacy#:~:text=Examples%20of%20digital%20health%20literacy,communicate%20with%20healthcare%20providers%20electronically.







 Understanding and managing cholesterol levels is crucial for maintaining heart health and reducing the risk of cardiovascular diseases. Here’s a detailed look at the factors that influence cholesterol and how you can take control:
Understanding and managing cholesterol levels is crucial for maintaining heart health and reducing the risk of cardiovascular diseases. Here’s a detailed look at the factors that influence cholesterol and how you can take control:

 Understanding cholesterol is crucial for managing cardiovascular health. Low-Density Lipoprotein (LDL) carries cholesterol from the liver to the cells, but when there’s an excess, it can accumulate in the walls of the arteries. High levels of LDL cholesterol are a significant risk factor for atherosclerosis, a condition where fatty deposits (plaques) build up in the arteries, reducing or blocking blood flow and potentially leading to heart disease or stroke.
Understanding cholesterol is crucial for managing cardiovascular health. Low-Density Lipoprotein (LDL) carries cholesterol from the liver to the cells, but when there’s an excess, it can accumulate in the walls of the arteries. High levels of LDL cholesterol are a significant risk factor for atherosclerosis, a condition where fatty deposits (plaques) build up in the arteries, reducing or blocking blood flow and potentially leading to heart disease or stroke.


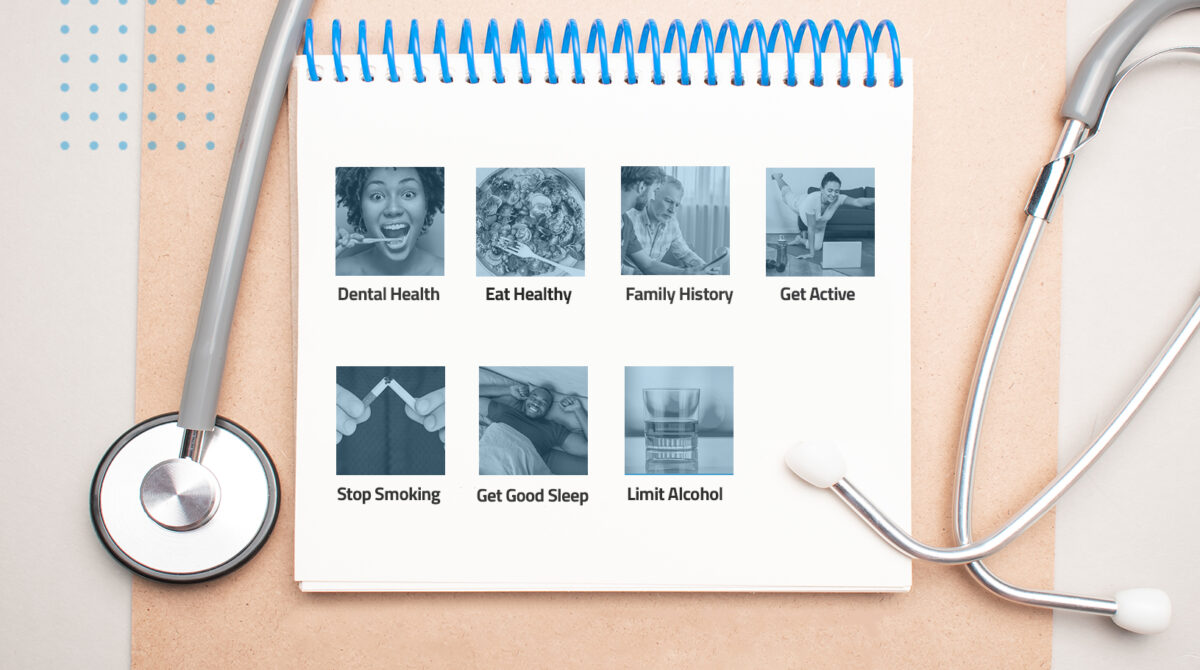
 Schedule Regular Check-Ups. Schedule annual physical exams to help detect health issues early, monitor chronic conditions, and update vaccinations. This will help you to create a personalized health plan and gain helpful preventive care advice from your health care providers..
Schedule Regular Check-Ups. Schedule annual physical exams to help detect health issues early, monitor chronic conditions, and update vaccinations. This will help you to create a personalized health plan and gain helpful preventive care advice from your health care providers..
 The majority of parents adhere to the CDC’s recommended immunization schedule for their children, ensuring protection against 14 potentially severe diseases before the child’s second birthday. Timely vaccination not only shields the vaccinated child but also safeguards those with compromised immune systems who may be vulnerable to illness. By immunizing children as advised, we create a shield of protection not just for them but for the broader community, contributing to public health efforts in preventing the spread of contagious diseases.
The majority of parents adhere to the CDC’s recommended immunization schedule for their children, ensuring protection against 14 potentially severe diseases before the child’s second birthday. Timely vaccination not only shields the vaccinated child but also safeguards those with compromised immune systems who may be vulnerable to illness. By immunizing children as advised, we create a shield of protection not just for them but for the broader community, contributing to public health efforts in preventing the spread of contagious diseases.